Did you know that changing hormone levels during menopause could be contributing to muscle pain, aches, and even spasms? The way you feel pain is influenced by many different factors including your genetic makeup and your mood. Read on to find out how hormones affect your experience of pain and which exercises and tips can help prevent cramping.
Find what you need quickly
Estrogen and pain sensitivity
Menopause impacts the way you feel pain by altering the processing of pain in your brain and spinal cord. Estrogen helps to regulate the release of your body’s natural painkillers, hormones also known as endorphins and enkephalins. When estrogen levels decline during the menopause transition, endorphins and enkephalins are released in smaller quantities. This is one reason why you may feel pain differently or more intensely after menopause and why aches and pains of all types can feel worse.
While it may seem that replacing estrogen would be an obvious solution, it doesn’t appear to be the case. Current research on this topic has found mixed conclusions as to whether the perception of pain is improved with HT use.
Estrogen and inflammation
Inflammation has been a hot topic in the health and wellness industry over recent years with anti-inflammatory diets, skincare, and lifestyle programs flooding the market. Inflammation is usually a helpful part of your body’s healing processes, but it can also cause problems with pain, swelling, and impaired healing in response to injuries or general wear and tear. Illnesses that are caused by uncontrolled inflammation include inflammatory bowel disease – such as ulcerative colitis and Crohn’s disease – and rheumatoid arthritis.
Estrogen has anti-inflammatory properties. Lower levels of estrogen after menopause are thought to be linked to increased levels of inflammation. As a result, any inflammation in your body can hang around for longer and be more difficult to control. Medical conditions caused by abnormal inflammation can flare up more frequently and more intensely, while injuries can take longer to heal. This is bad news for those annoying menopausal muscle aches and pains, whatever the cause.
Things that can help inflammation
- Exercise within your safe limits
- If you are taking up a new physical activity, get advice from a coach or physical education expert on how to get started safely
- Be sure to warm up and cool down properly to prevent injury when exercising
- Slow it down if you notice pain
- If you have any medical conditions associated with inflammation, speak to your healthcare provider to find out the best treatments for you
Watch out for osteoarthritis
Osteoarthritis is generally thought of as being an age-related wearing of the joints and is a frequent cause of joint pain, aches, pains, and muscle spasms. This common problem is caused by the deterioration of the bone and cartilage. Decreasing levels of estrogen at menopause are thought to have an impact. Symptoms include muscle pain, stiffness, swelling, and grinding or crunching sensations in the joints.
The combination of osteoarthritis, altered pain perception and increased levels of inflammation outside the joints can be particularly challenging for those going through menopause and beyond.
It is not possible to prevent osteoarthritis but you can take steps to improve symptoms and prevent it from getting any worse. Speak to your healthcare provider for advice on the best treatments for you.
Check your activity
If you are doing any strenuous or repetitive activity, think about ways you could ease the strain on your joints. If your job involves repeated heavy lifting or extended time on your feet, could you ask your occupational health team for lifting equipment or more regular breaks? If you run long distances, could you switch to a lower-impact form of exercise?
If you think you may have osteoarthritis, speak to your healthcare provider for advice.
Check your minerals, vitamins, and other hormones
Menopause muscle aches or spasms can be caused by many different medical conditions, some of which may be less obviously related to the bones and muscles.
Don’t be surprised if your healthcare provider asks you to have a blood test. They will be looking for conditions that can cause aches and pains, including:
- Thyroid problems
- Abnormal mineral levels, including calcium and magnesium
- Abnormal vitamin levels, including vitamin D
- Anemia
Improving posture and spinal health
In the age of video calls and desk jobs, most people could do with improving their posture, especially if struggling with back, neck, or shoulder pain. You may also notice the rounding of your shoulders or an unusual curvature of your spine at the neck, both of which can be part of the increasingly common upper crossed syndrome.
While it’s probably the last thing on your to-do list, it is worth paying some serious attention to your posture to keep your spine healthy for decades to come.
Tips for spine health and to reduce muscle aches
- Keep your TV or monitor raised – aim to have them at your eye level by hanging them on the wall or using a stand
- Choose a chair that provides good support to your lower back
- Keep the chair back upright – aim for a near-vertical backrest
- When seated, aim to have your knees slightly lower than your hips
- Use a footrest if it helps to ease any muscle aches and pains
- Take regular breaks to stretch and move around
- Take some form of exercise to support good posture – yoga and Pilates are good options
What exercises can help your posture?
Create a workspace that is mindful of your body, give yourself enough space, and position your accessories and tools, such as computers, optimally to reduce the incidence and severity of cramps.

The optimal office set up
It is recommended that you take a break from sitting at your desk every 30 – 40 minutes.
If you can’t leave your desk, here are some effective stretches and strengthening exercises that can relieve cramps and help you toward your fitness goals.
1. PREVENTING CRAMPS


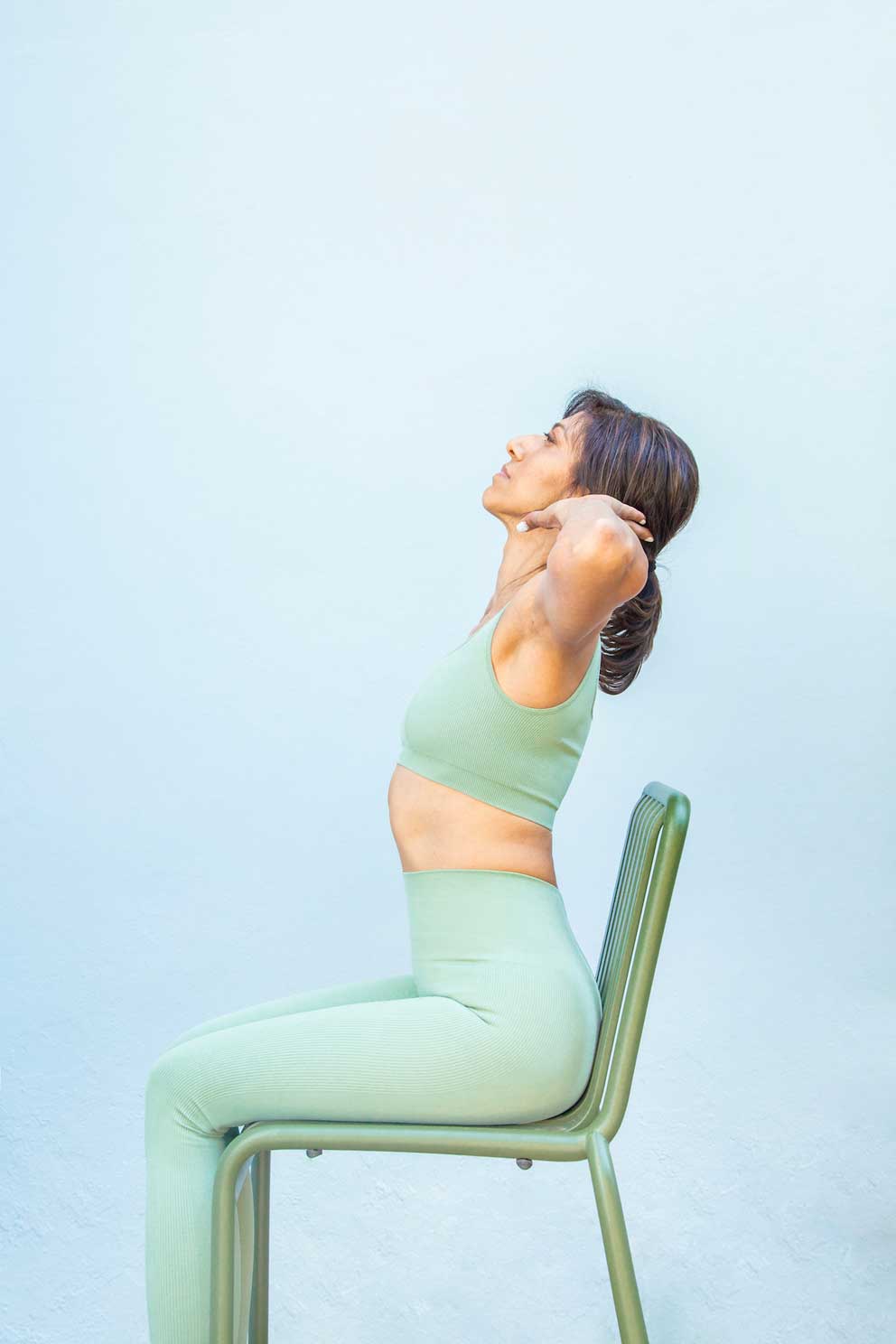
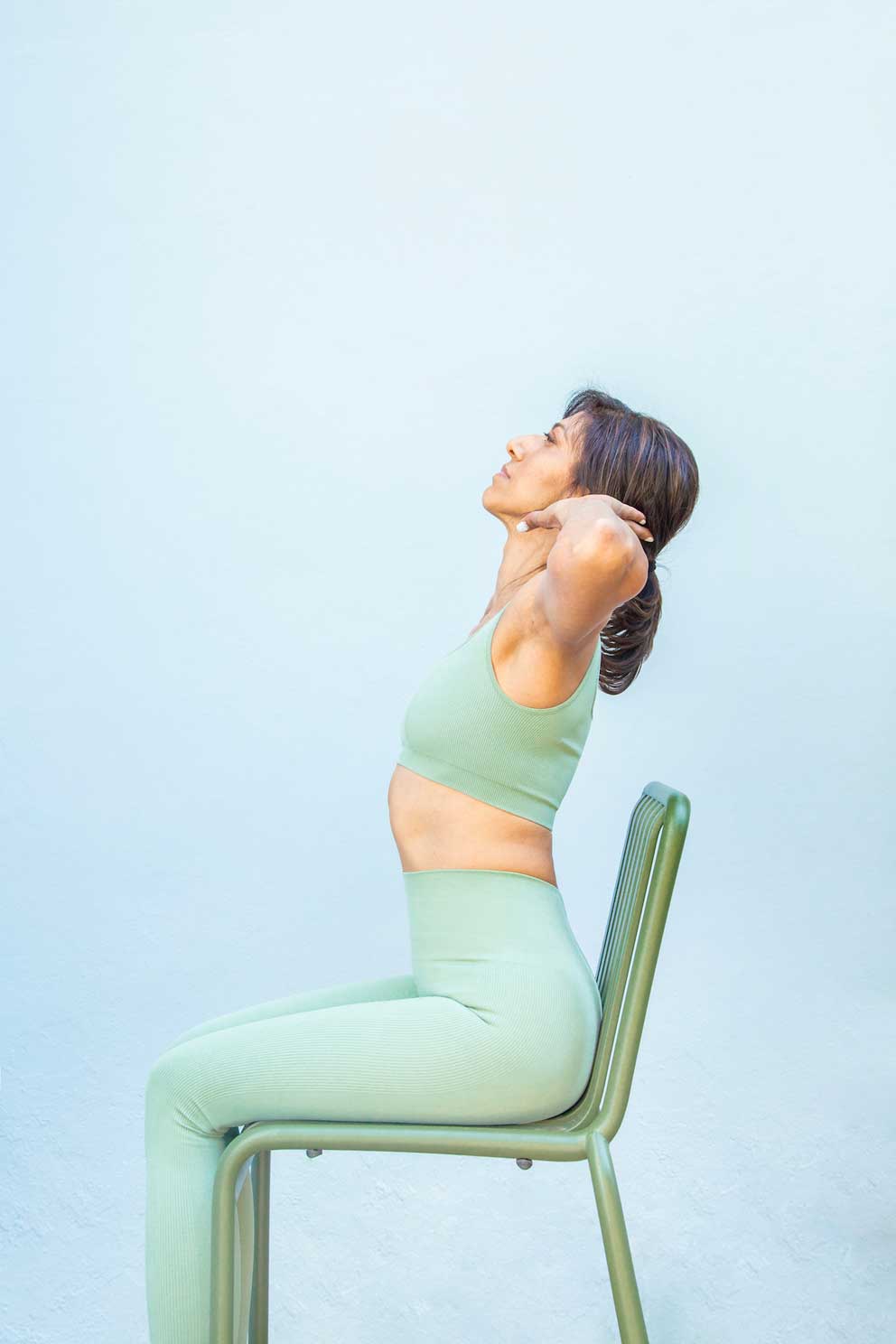




These stretches should be held for 20 seconds for three repetitions (3 x 20 secs). They help to activate and loosen the deep spinal muscles, shoulders, calves and hamstrings which are vulnerable to regular cramps.
2. BUILD STRENGTH




Medial leg lift – 10 repetitions in 3 sets (10 x 3). For progression, hold your legs for 10 seconds when they are directly out in front of you.
Knee to chest raises – 12 repetitions in 2 sets (12 x 2). For progression, on the leg extension, draw a star sign in the air with your toes, attempt this for as many repetitions as you are able.
Sleeping positions
It’s not just your daytime posture that contributes to aches and pains. Your sleep posture is just as important, especially when it comes to maintaining a healthy spine.
The best sleep position for spinal health is flat on your back, as this allows the spine to stay in an optimal alignment and reduces stress on the individual joints of the backbone. If you are a side sleeper, use pillows to support your head, separate your knees and support your upper shoulder if required.
Be sure to choose a mattress that works for you, and the right type of pillow for your preferred sleeping position.
Menopause muscle pain
Sometimes no underlying cause is found for your aches and pains, and they are simply put down to being part of menopause. If this is the case, your healthcare provider will be able to advise on the best treatments available for you.
Some find HT does seem to help them with general aches and menopausal muscle pain, but it isn’t a guaranteed solution. Evidence is still emerging and more research is needed.
HT has been proven to help with many other symptoms of menopause. Some of these – including sleep issues and feeling sad – can impact the way you experience pain. Find out more about HT risks and benefits.
When to see a healthcare provider
See your healthcare provider urgently if you have:
- Persistent muscle aches, pains, or spasms
- Any severe, worsening, or worrying pain
- Recently started or increased the dose of a statin (cholesterol medication)
- A history of kidney problems
- Any swelling or redness in your joints or limbs
- Any other symptoms or concerns
There are many different potential causes, many of which are treatable. Seeing your healthcare provider is the first step to getting a diagnosis. Sometimes persistent aches and pains can be caused by serious injuries. For example, from perimenopause onwards reduced estrogen levels mean that our bones become thinner and more prone to fractures. For some, this can cause osteoporosis which is a medical term for severe thinning of the bones. In some cases, bones are so thin that they can be fractured with low-impact injuries or no injury at all, known as fragility fractures.
Final word
While menopause muscle pain and aches are common at the time of menopause, it is still worth paying attention to any which become troublesome. Your healthcare provider will be able to help you understand what is causing them and if anything can be done to help.
Find out more about menopause on our blog or our symptoms library.